Journal Description
Journal of Personalized Medicine
Journal of Personalized Medicine
is an international, peer-reviewed, open access journal on personalized medicine, published monthly online by MDPI.
- Open Access— free for readers, with article processing charges (APC) paid by authors or their institutions.
- High Visibility: indexed within Scopus, SCIE (Web of Science), PubMed, PMC, Embase, and other databases.
- Journal Rank: JCR - Q2 (Medicine, General & Internal) CiteScore - Q2 (Medicine (miscellaneous))
- Rapid Publication: manuscripts are peer-reviewed and a first decision is provided to authors approximately 20.2 days after submission; acceptance to publication is undertaken in 1.9 days (median values for papers published in this journal in the first half of 2023).
- Recognition of Reviewers: reviewers who provide timely, thorough peer-review reports receive vouchers entitling them to a discount on the APC of their next publication in any MDPI journal, in appreciation of the work done.
Impact Factor:
3.4 (2022);
5-Year Impact Factor:
3.5 (2022)
Latest Articles
Pharmacogenetic Variants Associated with Fluoxetine Pharmacokinetics from a Bioequivalence Study in Healthy Subjects
J. Pers. Med. 2023, 13(9), 1352; https://doi.org/10.3390/jpm13091352 (registering DOI) - 01 Sep 2023
Abstract
Fluoxetine is one of the most prescribed antidepressants, yet it still faces challenges due to high intersubject variability in patient response. Mainly metabolized by the highly polymorphic gene CYP2D6, important differences in plasma concentrations after the same doses are found among individuals.
[...] Read more.
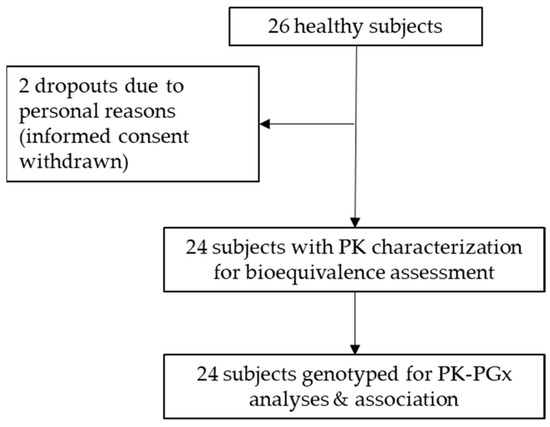
Fluoxetine is one of the most prescribed antidepressants, yet it still faces challenges due to high intersubject variability in patient response. Mainly metabolized by the highly polymorphic gene CYP2D6, important differences in plasma concentrations after the same doses are found among individuals. This study investigated the association of fluoxetine pharmacokinetics (PK) with pharmacogenetic variants. A bioequivalence crossover trial (two sequences, two periods) was conducted with fluoxetine 20 mg capsules, in 24 healthy subjects. Blood samples for fluoxetine determination were collected up to 72 h post-dose. Subjects were genotyped and single nucleotide variants (SNV) were selected using a candidate gene approach, and then associated with the PK parameters. Bioequivalence was confirmed for the test formulation. We found 34 SNV on 10 genes with a quantifiable impact on the PK of fluoxetine in the randomized controlled trial. Out of those, 29 SNVs belong to 7 CYPs (CYP1A2, CYP2B6, CYP2C9, CYP2C19, CYP2D6, CYP3A4, CYP3A5), and 5 SNVs to 3 genes impacting the pharmacodynamics and efficacy of fluoxetine (SLC6A4, TPH1, ABCB1). Moreover, decreased/no function SNVs of CYP2D6 (rs1065852, rs28371703, rs1135840) and CYP2C19 (rs12769205) were confirmed phenotypically. Our research contributes to deepening the catalog of genotype-phenotype associations in pharmacokinetics, aiming to increase pharmacogenomics knowledge for rational treatment schemes of antidepressants.
Full article
(This article belongs to the Special Issue Pharmacogenetics and Pharmacogenomics in Personalized Medicine)
►
Show Figures
Open AccessArticle
Persistent Endothelial Lung Damage and Impaired Diffusion Capacity in Long COVID
by
, , , , , , , , , , , , , , and
J. Pers. Med. 2023, 13(9), 1351; https://doi.org/10.3390/jpm13091351 (registering DOI) - 31 Aug 2023
Abstract
Since the beginning of the pandemic, both COVID-19-associated coagulopathy biomarkers and a plethora of endothelial biomarkers have been proposed and tested as prognostic tools of severity and mortality prediction. As the pandemic is gradually being controlled, attention is now focusing on the long-term
[...] Read more.
Since the beginning of the pandemic, both COVID-19-associated coagulopathy biomarkers and a plethora of endothelial biomarkers have been proposed and tested as prognostic tools of severity and mortality prediction. As the pandemic is gradually being controlled, attention is now focusing on the long-term sequelae of COVID-19. In the present study, we investigated the role of endothelial activation/dysfunction in long COVID syndrome. This observational study included 68 consecutive long COVID patients and a healthy age and sex-matched control group. In both groups, we measured 13 endothelial biomarkers. Moreover, in the long COVID patients, we evaluated fatigue and dyspnea severity, lung diffusion capacity (DLCO), and the 6-minute walk (6MWT) test as measures of functional capacity. Our results showed that markers of endothelial activation/dysfunction were higher in long COVID patients, and that soluble intracellular adhesion molecule 1 (sICAM-1) and soluble vascular adhesion molecule 1 (sVCAM-1) negatively correlated with lung diffusion and functional capacity (sICAM-1 vs. DLCO, r = −0.306, p = 0.018; vs. 6MWT, r = −0.263, p = 0.044; and sVCAM-1 vs. DLCO, r= −0.346, p = 0.008; vs. 6MWT, r = −0.504, p < 0.0001). In conclusion, evaluating endothelial biomarkers alongside clinical tests might yield more specific insights into the pathophysiological mechanisms of long COVID manifestations.
Full article
(This article belongs to the Special Issue Personalized Medicine for Post COVID and Long COVID)
Open AccessArticle
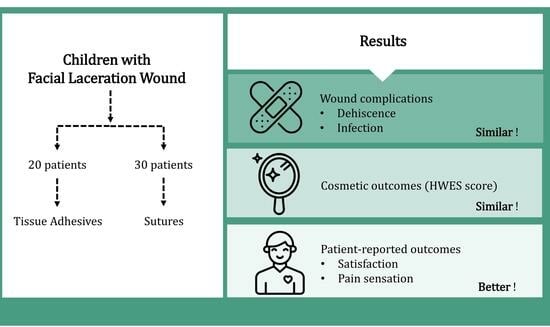
Comparative Evaluation of Tissue Adhesives and Sutures in the Management of Facial Laceration Wounds in Children
by
, , , , , and
J. Pers. Med. 2023, 13(9), 1350; https://doi.org/10.3390/jpm13091350 - 31 Aug 2023
Abstract
Background: This study evaluated tissue adhesives in comparison to sutures for treating facial lacerations in children. Methods: We retrospectively analyzed data from September 2017 to August 2022 involving pediatric facial lacerations managed with either tissue adhesives or sutures. Results: Among 50 children, 20
[...] Read more.
Background: This study evaluated tissue adhesives in comparison to sutures for treating facial lacerations in children. Methods: We retrospectively analyzed data from September 2017 to August 2022 involving pediatric facial lacerations managed with either tissue adhesives or sutures. Results: Among 50 children, 20 received tissue adhesives, and 30 received sutures. Both methods showed comparable outcomes in terms of wound complications such as dehiscence (adjusted odds ratio = 1.56, 95% CI = 0.08–31.25) and infection (adjusted odds ratio = 2.17, 95% CI = 0.08–58.80). The cosmetic outcomes, assessed using the Hollander Wound Evaluation Score, were also consistent between groups (adjusted beta = −0.55, 95% CI = −1.15–0.05). Notably, those treated with tissue adhesives reported greater satisfaction (adjusted beta = 1.13, 95% CI = 0.63 −1.63) and experienced significantly less pain (adjusted beta = −3.03, 95% CI = −4.15–−1.90). Conclusions: Both techniques displayed similar rates of infection, dehiscence, and cosmetic outcomes. However, tissue adhesives were associated with increased patient comfort, especially in terms of reduced pain and greater satisfaction.
Full article
(This article belongs to the Special Issue Implications for Personalized Plastic, Aesthetic and Reconstructive Surgery)
►▼
Show Figures
Graphical abstract
Open AccessReview
Association of Broad-Spectrum Antibiotic Therapy and Vitamin E Supplementation with Vitamin K Deficiency-Induced Coagulopathy: A Case Report and Narrative Review of the Literature
by
, , , , , , , , , and
J. Pers. Med. 2023, 13(9), 1349; https://doi.org/10.3390/jpm13091349 - 31 Aug 2023
Abstract
Vitamin K is a lipid-soluble vitamin that is normally maintained within appropriate levels by means of dietary intake and bacterial production in the intestinal microflora. It holds a central role in coagulation homeostasis, and thus its depletion leads to hypocoagulation and haemorrhagic diathesis.
[...] Read more.
Vitamin K is a lipid-soluble vitamin that is normally maintained within appropriate levels by means of dietary intake and bacterial production in the intestinal microflora. It holds a central role in coagulation homeostasis, and thus its depletion leads to hypocoagulation and haemorrhagic diathesis. The association of antibiotic therapy and vitamin E supplementation with vitamin K deficiency was previously described in animal experiments, clinical studies, and case reports. Broad-spectrum antibiotic therapy potentially leads to intestinal microflora dysbiosis and restriction of vitamin K-producing bacterial populations, resulting in decreased vitamin K levels, whereas antibiotics of the cephalosporin class with 1-N-methyl-5-thiotetrazole (NMTT) or 2-methyl-1,3,4-thiadiazole (MTD) side groups inhibit vitamin K function. Vitamin E supplementation interferes with both the bioavailability and function of vitamin K, yet its mechanisms are not fully understood. We present the case of a 45-year-old male patient, with a history of epilepsy and schizophrenia, catatonically incapacitated and immobilised, who was hospitalised in our centre for the investigation and management of aspiration pneumonia. He demonstrated a progressively worsening prolongation of international normalised ratio (INR), which was attributed to both broad-spectrum antibiotic therapy and vitamin E supplementation and was reversed upon administration of vitamin K. We highlight the need for close monitoring of coagulation parameters in patients receiving broad-spectrum antibiotic therapy, especially those with underlying malnutritive or malabsorptive conditions, and we further recommend the avoidance of NMTT- or MTD-containing antibiotics or vitamin E supplementation, unless absolutely necessary, in those patients.
Full article
(This article belongs to the Special Issue Pulmonary Medicine: Diagnosis and Personalized Treatment)
►▼
Show Figures
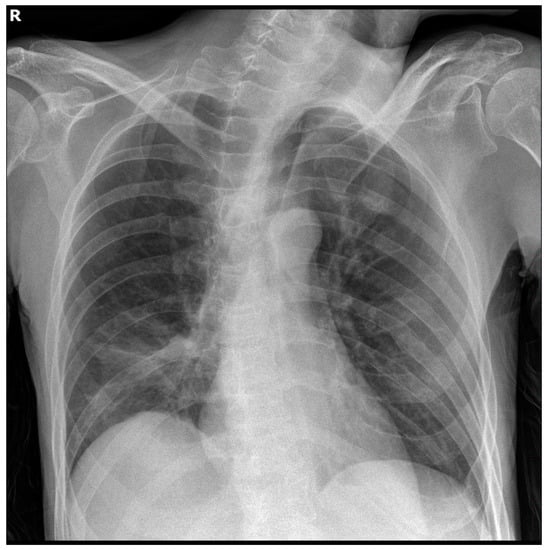
Figure 1
Open AccessArticle
Cardiac Troponin I but Not N-Terminal Pro-B-Type Natriuretic Peptide Predicts Outcomes in Cardiogenic Shock
by
, , , , , , , , , and
J. Pers. Med. 2023, 13(9), 1348; https://doi.org/10.3390/jpm13091348 - 31 Aug 2023
Abstract
This study investigates the prognostic value of cardiac troponin I (cTNI) and N-terminal pro-B-type natriuretic peptide (NT-proBNP) levels in patients with cardiogenic shock (CS). Data regarding the prognostic value of cardiac biomarkers in CS is scarce, furthermore, most studies were restricted to CS
[...] Read more.
This study investigates the prognostic value of cardiac troponin I (cTNI) and N-terminal pro-B-type natriuretic peptide (NT-proBNP) levels in patients with cardiogenic shock (CS). Data regarding the prognostic value of cardiac biomarkers in CS is scarce, furthermore, most studies were restricted to CS patients with acute myocardial infarction (AMI). Therefore, consecutive patients with CS from 2019 to 2021 were included. Blood samples were retrieved from day of disease onset (day 1) and on days 2, 3 and 4 thereafter. The prognostic value of cTNI and NT-proBNP levels was tested for 30-day all-cause mortality. Statistical analyses included univariable t-tests, Spearman’s correlations, Kaplan–Meier analyses and multivariable Cox proportional regression analyses. A total of 217 CS patients were included with an overall rate of all-cause mortality of 56% at 30 days. CTNI was able to discriminate 30-day non-survivors (area under the curve (AUC) = 0.669; p = 0.001), whereas NT-proBNP (AUC = 0.585; p = 0.152) was not. The risk of 30-day all-cause mortality was higher in patients with cTNI levels above the median (70% vs. 43%; log rank p = 0.001; HR = 2.175; 95% CI 1.510–3.132; p = 0.001), which was observed both in patients with (71% vs. 49%; log rank p = 0.012) and without AMI-related CS (69% vs. 40%; log rank p = 0.005). The prognostic impact of cTNI was confirmed after multivariable adjustment (HR = 1.915; 95% CI 1.298–2.824; p = 0.001). In conclusion, cTNI—but not NT-proBNP—levels discriminated 30-day all-cause mortality in CS patients.
Full article
(This article belongs to the Special Issue Percutaneous Management of Complex Coronary Artery Disease—Updates on Clinical Outcomes, Management Strategies and Novel Techniques)
►▼
Show Figures
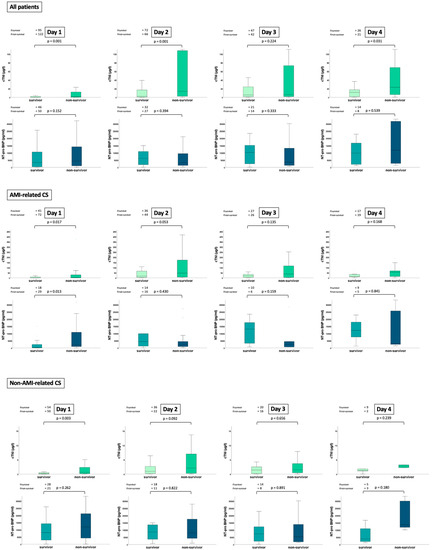
Figure 1
Open AccessBrief Report
TNFα rs1800629 Polymorphism and Response to Anti-TNFα Treatment in Behçet Syndrome: Data from an Italian Cohort Study
by
, , , , , and
J. Pers. Med. 2023, 13(9), 1347; https://doi.org/10.3390/jpm13091347 - 31 Aug 2023
Abstract
Tumor Necrosis Factor-alpha (TNFα) rs1800629 (-308G>A) is a single nucleotide polymorphism (SNP) related to variable responses to anti-TNFα therapy. This therapy is efficient in severe and refractory manifestation of Behçet syndrome (BS), an auto-inflammatory systemic vasculitis. We investigated (1) the
[...] Read more.
Tumor Necrosis Factor-alpha (TNFα) rs1800629 (-308G>A) is a single nucleotide polymorphism (SNP) related to variable responses to anti-TNFα therapy. This therapy is efficient in severe and refractory manifestation of Behçet syndrome (BS), an auto-inflammatory systemic vasculitis. We investigated (1) the association between rs1800629 genotypes and responses to therapy and (2) the correlation between SNP and clinical patterns in a cohort of 74 BS Italian patients receiving anti-TNFα therapy with a follow-up of at least 12 months. The rs1800629 was genotyped through amplification, direct sequencing and bioinformatics analyses. The rs1800629 GG and GA genotypes were assessed as predictors of outcomes dividing the patients between therapy responders and non-responders. The rs1800629 GG and GA genotypes were found, respectively, in 59/74 (79.7%) and 15/74 BS patients (21.3%) (p < 0.05). We identified 16/74 (21.9%) non-responder patients, of which 9/16 (56.3%) showed the GG genotype and 7/16 (43.7%) the GA genotype. A total of 50/58 (86.2%) responder patients showed the GG genotype, and 8/58 (13.8%) the GA genotype (p < 0.05). The percentage of non-responder females (68.8%) was significantly higher than non-responder males (31.2%) (p < 0.05). No correlation between SNP and clinical patterns was observed. To successfully include rs1800629 as a predictive biomarker of TNFα inhibitor response, genome-wide association studies in larger, well-characterised cohorts are required.
Full article
(This article belongs to the Section Pharmacogenetics)
Open AccessFeature PaperArticle
Impact of the Allergic Therapeutic Adherence in Children with Allergic Rhinitis and ADHD: A Pilot Study
by
, , , , , , , , and
J. Pers. Med. 2023, 13(9), 1346; https://doi.org/10.3390/jpm13091346 - 31 Aug 2023
Abstract
Background: Allergic rhinitis (AR) is the most common chronic allergic disease in children. Several studies have shown an association between attention deficit hyperactivity disorder (ADHD) and allergies, especially AR. Patients with ADHD usually have poor therapeutic adherence, and untreated AR symptoms may worsen
[...] Read more.
Background: Allergic rhinitis (AR) is the most common chronic allergic disease in children. Several studies have shown an association between attention deficit hyperactivity disorder (ADHD) and allergies, especially AR. Patients with ADHD usually have poor therapeutic adherence, and untreated AR symptoms may worsen the quality of life of patients. Methods: The aim of our study was to analyse therapeutic adherence in patients with ADHD and AR and estimate the impact of the adherence on ADHD symptoms. Total Nasal Symptoms Score (TNSS), Paediatric or Adolescent Rhinoconjunctivitis Quality of Life Questionnaire (PRQLQ 6–12 years; ARQLQ 13–17 years), Swanson, Nolan, and Pelham version IV scale (SNAP-IV), and Medication Assessment Questionnaire (MGL MAQ) were recorded. Results: In the AR-ADHD group, a positive correlation between TNSS and SNAP-IV subscales was found: worse AR symptoms were related to a negative effect on ADHD scores. AR-ADHD patients with better ADHD therapeutic adherence showed higher AR symptoms and higher oppositional defiant disorder scores in the SNAP-IV questionnaire. Conclusions: Our results suggest that better adherence to AR therapy (oral antihistamines and/or intranasal corticosteroids, INCS) is associated with a reduction in inattention symptoms in children with ADHD. This data could prove to be fundamental for the psychic outcome of these patients.
Full article
(This article belongs to the Section Clinical Medicine, Cell, and Organism Physiology)
Open AccessBrief Report
Intraoperative Fluorescent Ureter Visualization in Complex Laparoscopic or Robotic-Assisted Gynecologic Surgery
by
, , , , , , and
J. Pers. Med. 2023, 13(9), 1345; https://doi.org/10.3390/jpm13091345 - 31 Aug 2023
Abstract
This study aimed to demonstrate the feasibility of ureteral navigation using intraoperative indocyanine green (ICG) and near-infrared fluorescence (NIRF) imaging during complex laparoscopic or robot-assisted gynecologic surgery (LRAGS). Twenty-six patients at high risk of ureteral injury with complex pelvic pathology (CPP) due to
[...] Read more.
This study aimed to demonstrate the feasibility of ureteral navigation using intraoperative indocyanine green (ICG) and near-infrared fluorescence (NIRF) imaging during complex laparoscopic or robot-assisted gynecologic surgery (LRAGS). Twenty-six patients at high risk of ureteral injury with complex pelvic pathology (CPP) due to pelvic organ prolapse (POP), multiple myomas, large intraligamentary or cervical myoma, severe pelvic adhesions, or cervical atresia underwent LRAGS. All patients underwent cystoscopic intraureteral ICG instillation before LRAGS and ureteral navigation under NIRF imaging intraoperatively. Both ureteral pathways were identified from the pelvic brim downwards through NIRF imaging in all patients, even though some were not visualized under the white light mode. The fluorescent ureters were visualized immediately after the beginning of surgery and typically lasted for >5 h during surgery. There were no cases of iatrogenic ureteral injury. The hemoglobin decrement was 1.47 ± 1.13 g/dL, and no transfusion was required. In our study, both ureters in all patients were identified with ICG-NIRF imaging during LRAGS, and these techniques made surgeries easier and safer. Despite the CPP, there was no ureteral injury or transfusion following surgery. Further prospective studies are needed to introduce intraoperative ureteral guidelines for ICG-NIRF imaging during LRAGS with CPP.
Full article
(This article belongs to the Special Issue Gynecological Surgery: Current Perspectives and Future Challenges)
►▼
Show Figures
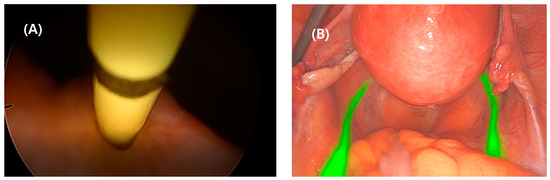
Figure 1
Open AccessCase Report
Successful Caesarean Section on Ticagrelor Treatment One Day after Primary Percutaneous Coronary Intervention
by
, , , , , , , , and
J. Pers. Med. 2023, 13(9), 1344; https://doi.org/10.3390/jpm13091344 - 30 Aug 2023
Abstract
Caesarean section is a challenging intervention in patients treated with dual antiplatelet therapy. We present a case of a 32-year-old pregnant woman experiencing large acute myocardial infarction (MI) of the anterolateral wall, complicated by cardiogenic shock in the 38th week of pregnancy, and
[...] Read more.
Caesarean section is a challenging intervention in patients treated with dual antiplatelet therapy. We present a case of a 32-year-old pregnant woman experiencing large acute myocardial infarction (MI) of the anterolateral wall, complicated by cardiogenic shock in the 38th week of pregnancy, and treated with drug-eluting stent implantation and dual antiplatelet therapy (DAPT) consisting of aspirin and ticagrelor. Less than 24 h after the MI delivery started, an urgent Caesarean section was indicated. As multiplate aggregometry testing showed a relatively insufficient level of ticagrelor platelet inhibition and a moderate level of aspirin platelet inhibition, a Caesarean section was performed without discontinuation of ticagrelor, which was decided due to the need for emergency surgery. Local hemostatic measures including administration of tranexamic acid were applied. The patient did not experience excessive bleeding. A healthy male baby was born. To the best of our knowledge, this is the first reported case of surgery in pregnant women treated with DAPT without ticagrelor discontinuation.
Full article
(This article belongs to the Section Personalized Therapy and Drug Delivery)
►▼
Show Figures

Figure 1
Open AccessArticle
High Frequency of Osteophytes Detected by High-Resolution Ultrasound at the Finger Joints of Asymptomatic Factory Workers
by
, , , , , , , , and
J. Pers. Med. 2023, 13(9), 1343; https://doi.org/10.3390/jpm13091343 - 30 Aug 2023
Abstract
Hand Osteoarthritis (HOA) is a frequently occurring musculoskeletal disease that impacts health. Diagnostic criteria often incorporate osteophytes documented through imaging procedures. Radiographic imaging is considered the gold standard; however, more sensitive and safer methods like ultrasound imaging are becoming increasingly important. We conducted
[...] Read more.
Hand Osteoarthritis (HOA) is a frequently occurring musculoskeletal disease that impacts health. Diagnostic criteria often incorporate osteophytes documented through imaging procedures. Radiographic imaging is considered the gold standard; however, more sensitive and safer methods like ultrasound imaging are becoming increasingly important. We conducted a population-based cross-sectional study to examine the prevalence, grade, and pattern of osteophytes using high-resolution ultrasound investigation. Factory workers were recruited on-site for the study. Each participant had 26 finger joints examined using ultrasonography to grade the occurrence of osteophytes on a semi-quantitative scale ranging from 0–3, where higher scores indicate larger osteophytes. A total of 427 participants (mean age 53.5 years, range 20–79 years) were included, resulting in 11,000 joints scored. At least one osteophyte was found in 4546 out of 11,000 (41.3%) joints or in 426 out of 427 (99.8%) participants, but only 5.0% (553) of the joints showed grade 2 or 3 osteophytes. The total osteophyte sum score increased by 0.18 per year as age increased (p < 0.001). The distal interphalangeal joints were the most commonly affected, with 61%, followed by the proximal interphalangeal joints with 48%, carpometacarpal joint 1 with 39%, and metacarpophalangeal joints with 16%. There was no observed impact of gender or workload. In conclusion, ultrasound imaging proves to be a practical screening tool for osteophytes and HOA. Grade 1 osteophytes are often detected in the working population through ultrasound assessments and their incidence increases with age. The occurrence of grade 2 or 3 osteophytes is less frequent and indicates the clinical presence of HOA. Subsequent evaluations are imperative to ascertain the predictive significance of early osteophytes.
Full article
(This article belongs to the Topic Diagnosis, Management, and Prognostic Assessment of Chronic Disease)
►▼
Show Figures

Figure 1
Open AccessArticle
The Relationship of Cognitive Dysfunction with Inflammatory Markers and Carotid Intima Media Thickness in Schizophrenia
J. Pers. Med. 2023, 13(9), 1342; https://doi.org/10.3390/jpm13091342 - 30 Aug 2023
Abstract
Objectives: Schizophrenia is a devastating and chronic mental disorder that affects 1% of the population worldwide. It is also associated with cognitive dysfunction and cardiovascular risk factors. The aim of this study is to investigate the relationship between cognitive impairment and some inflammatory
[...] Read more.
Objectives: Schizophrenia is a devastating and chronic mental disorder that affects 1% of the population worldwide. It is also associated with cognitive dysfunction and cardiovascular risk factors. The aim of this study is to investigate the relationship between cognitive impairment and some inflammatory markers and carotid intima-media thickness (CIMT) in schizophrenia. Methods: The participants of this study were 51 schizophrenia and 57 healthy controls (HC). The Positive and Negative Syndrome Scale (PANSS) was used for severity of illness, and the Montreal Cognitive Assessment Scale (MoCA) was used for cognitive functioning. The MoCA scores, some biochemical and inflammatory markers, and CIMT were compared between schizophrenia and HC groups. Results: Of the patients with schizophrenia, 11 were women (21.6%), and 40 were men (78.4%). MoCA scores were lower, and levels of NLR, MLR, PLR, SII, CRP, ESR, and CIMT were higher in schizophrenia compared to the HC group (respectively; p < 0.001, p < 0.001, p = 0.035, p = 0.008, p = 0.002, p < 0.001, p < 0.001, p < 0.001). In the schizophrenia group, there was no correlation between MoCA and inflammatory markers. MoCA and CIMT had a significant negative and moderate correlation (p < 0.001). Conclusions: This is the first study to show the relationship between cognitive impairment and CIMT in schizophrenia. In this study, NLR, MLR, PLR, SII, CRP, and ESR markers were higher in schizophrenia compared to HC, indicating inflammation. Our finding of elevated CIMT in schizophrenia suggests that there may be an atherosclerotic process along with the inflammatory process. The finding of a positive correlation between cognitive impairment and CIMT may be promising for new therapies targeting the atherosclerotic process in the treatment of cognitive impairment.
Full article
(This article belongs to the Section Disease Biomarker)
►▼
Show Figures
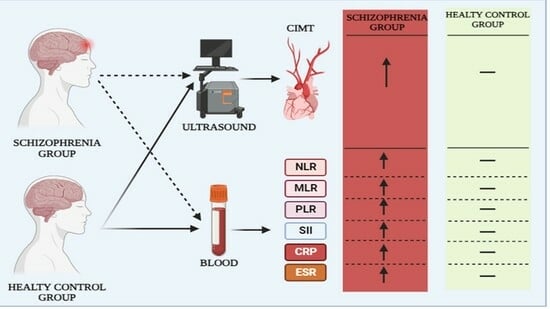
Graphical abstract
Open AccessArticle
Correlation between Severity of Idiopathic Epiretinal Membrane and Irvine–Gass Syndrome
J. Pers. Med. 2023, 13(9), 1341; https://doi.org/10.3390/jpm13091341 - 30 Aug 2023
Abstract
A higher risk of pseudophakic cystoid macular edema (PCME) has been reported in patients with preoperative idiopathic epiretinal membrane (ERM); however, whether the formation of PCME depends on the grade of ERM has not been well established. We conducted a retrospective case–control study
[...] Read more.
A higher risk of pseudophakic cystoid macular edema (PCME) has been reported in patients with preoperative idiopathic epiretinal membrane (ERM); however, whether the formation of PCME depends on the grade of ERM has not been well established. We conducted a retrospective case–control study of 87 eyes of 78 patients who were preoperatively diagnosed with idiopathic ERM and had undergone cataract surgery. Patients were divided into two groups: PCME and non-PCME groups. After cataract surgery, the ERM status was graded using the Gass and Govetto classifications. Both the central macular thickness (CMT) and ERM grade increased after surgery, and higher preoperative CMT and ERM grades were found in the PCME group. The association between higher-grade ERM and the development of PCME was significant in the Govetto classification (grade 2, odds ratio (OR): 3.13; grade 3, OR: 3.93; and grade 4, OR: 16.07). The study results indicate that close attention should be given to patients with ERM with the presence of an ectopic inner foveal layer before cataract surgery.
Full article
(This article belongs to the Section Clinical Medicine, Cell, and Organism Physiology)
Open AccessArticle
Carpal Tunnel Syndrome Associated with Immune Checkpoint Inhibitors
by
, , , , , , and
J. Pers. Med. 2023, 13(9), 1340; https://doi.org/10.3390/jpm13091340 - 30 Aug 2023
Abstract
Immune checkpoint inhibitors (ICIs) have transformed the therapeutic approach to diverse malignancies, leading to substantial enhancements in patient prognosis. However, along with their benefits, ICIs also increase the incidence of immune-related adverse events (irAEs). In the present paper, we highlight four cases of
[...] Read more.
Immune checkpoint inhibitors (ICIs) have transformed the therapeutic approach to diverse malignancies, leading to substantial enhancements in patient prognosis. However, along with their benefits, ICIs also increase the incidence of immune-related adverse events (irAEs). In the present paper, we highlight four cases of carpal tunnel syndrome (CTS) as an uncommon manifestation of toxicity induced by ICIs. Although diagnosed with different malignancies, the patients were undergoing ICI therapy when they developed CTS-consistent side effects accompanied by severe neuropathy. Prompt treatment with corticosteroids, intravenous immunoglobulins, or methotrexate resulted in complete symptomatic relief for all patients. This article therefore emphasizes the importance of recognizing and managing rare adverse events associated with ICI use to ensure optimal patient care.
Full article
(This article belongs to the Special Issue Novel Advances in Cancer Immunotherapy and Targeted Therapy)
►▼
Show Figures
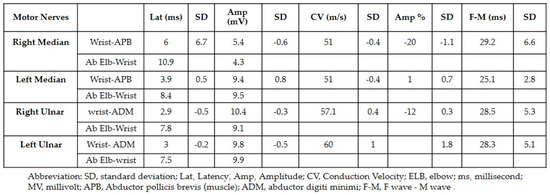
Figure 1
Open AccessReview
Antibody–Drug Conjugates for the Treatment of Renal Cancer: A Scoping Review on Current Evidence and Clinical Perspectives
by
, , , , and
J. Pers. Med. 2023, 13(9), 1339; https://doi.org/10.3390/jpm13091339 - 30 Aug 2023
Abstract
Antibody–drug conjugates (ADCs) are complex chemical structures composed of a monoclonal antibody, serving as a link to target cells, which is conjugated with a potent cytotoxic drug (i.e., payload) through a chemical linker. Inspired by Paul Ehrlich’s concept of the ideal anticancer drug
[...] Read more.
Antibody–drug conjugates (ADCs) are complex chemical structures composed of a monoclonal antibody, serving as a link to target cells, which is conjugated with a potent cytotoxic drug (i.e., payload) through a chemical linker. Inspired by Paul Ehrlich’s concept of the ideal anticancer drug as a “magic bullet”, ADCs are also highly specific anticancer agents, as they have been demonstrated to recognize, bind, and neutralize cancer cells, limiting injuries to normal cells. ADCs are among the newest pharmacologic breakthroughs in treating solid and hematologic malignancies. Indeed, in recent years, various ADCs have been approved by the Food and Drug Administration and European Medicines Agency for the treatment of several cancers, resulting in a “practice-changing” approach. However, despite these successes, no ADC is approved for treating patients affected by renal cell carcinoma (RCC). In the present paper, we thoroughly reviewed the current literature and summarized preclinical studies and clinical trials that evaluated the activity and toxicity profile of ADCs in RCC patients. Moreover, we scrutinized the potential causes that, until now, hampered the therapeutical success of ADCs in those patients. Finally, we discussed novel strategies that would improve the development of ADCs and their efficacy in treating RCC patients.
Full article
(This article belongs to the Section Methodology, Drug and Device Discovery)
►▼
Show Figures
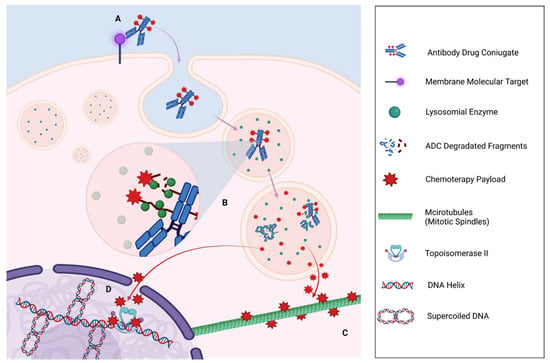
Figure 1
Open AccessArticle
An Efficient, Lightweight, Tiny 2D-CNN Ensemble Model to Detect Cardiomegaly in Heart CT Images
J. Pers. Med. 2023, 13(9), 1338; https://doi.org/10.3390/jpm13091338 - 30 Aug 2023
Abstract
Cardiomegaly is a significant global health concern, especially in developing nations. Although advanced clinical care is available for newly diagnosed patients, many in resource-limited regions face late diagnoses and consequent increased mortality. This challenge is accentuated by a scarcity of radiography equipment and
[...] Read more.
Cardiomegaly is a significant global health concern, especially in developing nations. Although advanced clinical care is available for newly diagnosed patients, many in resource-limited regions face late diagnoses and consequent increased mortality. This challenge is accentuated by a scarcity of radiography equipment and radiologists. Hence, we propose the development of a computer-aided diagnostic (CAD) system, specifically a lightweight, tiny 2D-CNN ensemble model, to facilitate early detection and, potentially, reduce mortality rates. Deep learning, with its subset of convolutional neural networks (CNN), has shown potential in visual applications, especially in medical image diagnosis. However, traditional deep CNNs often face compatibility issues with object-oriented human factor technology. Our proposed model aims to bridge this gap. Using CT scan images sourced from the Mendeley data center, our tiny 2D-CNN ensemble learning model achieved an accuracy of 96.32%, offering a promising tool for efficient and accurate cardiomegaly detection.
Full article
(This article belongs to the Section Methodology, Drug and Device Discovery)
►▼
Show Figures
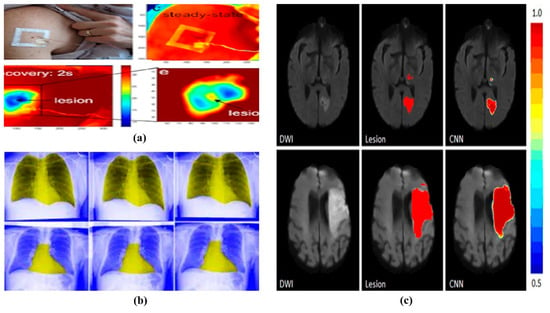
Figure 1
Open AccessSystematic Review
Impact of COVID-19 on Fetal Outcomes in Pregnant Women: A Systematic Review and Meta-Analysis
J. Pers. Med. 2023, 13(9), 1337; https://doi.org/10.3390/jpm13091337 - 30 Aug 2023
Abstract
Background: Coronavirus disease (COVID-19) is a pandemic causing respiratory symptoms, taste alterations, olfactory disturbances, and cutaneous, cardiovascular, and neurological manifestations. Recently, research interest has shifted to reproductive health to understand the factors predisposing to COVID-19 infection in pregnancy, the consequences of the infection
[...] Read more.
Background: Coronavirus disease (COVID-19) is a pandemic causing respiratory symptoms, taste alterations, olfactory disturbances, and cutaneous, cardiovascular, and neurological manifestations. Recently, research interest has shifted to reproductive health to understand the factors predisposing to COVID-19 infection in pregnancy, the consequences of the infection on the fetus and on the mother, and possible vertical transmission through the placenta. Pregnancy does not increase the risk of SARS-CoV-2 infection, according to studies. However, contrary to non-pregnant women, pregnancy worsens the clinical outcome of COVID-19. Studies investigating the effects of COVID-19 on pregnancy women are heterogeneous, and the results are often conflicting. Objectives: The goal of the current work was to offer a thorough and up-to-date systematic review of, and meta-analysis on, the impact of COVID-19 on ovarian function, pregnancy, and fetal outcomes. Search strategy: This meta-analysis (PROSPERO n. CRD42023456904) was conducted using the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) protocols. The search for relevant material was conducted using PubMed, Scopus, Cochrane, and Embase databases, through to 15 December 2022. Selection criteria: Original articles on fertile pregnant women or women attempting to become pregnant, with an active case of, or history of, SARS-CoV-2 infection were included, and reproductive function was compared to that of uninfected women. Data collection and analysis: The effects of COVID-19 on female reproductive function, particularly ovarian function, the profile of female sex hormones, pregnancy outcomes and fetal outcomes were the focus of our search. Quantitative analysis was performed with Comprehensive Meta-Analysis Software. The standard difference of the mean was calculated for the statistical comparison between cases and controls. Cochran’s Q test and heterogeneity (I2) indexes were used to assess statistical heterogeneity. Sensitivity analysis and publication bias tests were also performed. Main Results: Twenty-eight articles met our inclusion criteria, for a total of 27,383 patients pregnant or looking to have offspring, with active or anamnestic COVID-19, and 1,583,772 uninfected control women. Our study revealed that there was no significant difference between COVID-19 patients and the control group in terms of maternal characteristics such as age, body mass index (BMI) and comorbidities that could affect pregnancy and fetal outcomes. The risk of a miscarriage or Cesarean delivery was significantly lower, while the risk of fetal death or premature delivery was significantly higher in COVID-19 patients than in the controls. None of the included studies evaluated hormonal profiles or investigated the presence of infertility. Conclusions: Maternal comorbidities, age, and BMI do not raise the risk of COVID-19. However, pregnant women with COVID-19 had a lower risk of miscarriage and Cesarean delivery, possibly because of better prenatal care and high levels of observation during labor. COVID-19 during pregnancy increases the risk of fetal death and premature delivery.
Full article
(This article belongs to the Special Issue Post Sequelae of COVID-19: Focus on Metabolic Alterations)
►▼
Show Figures
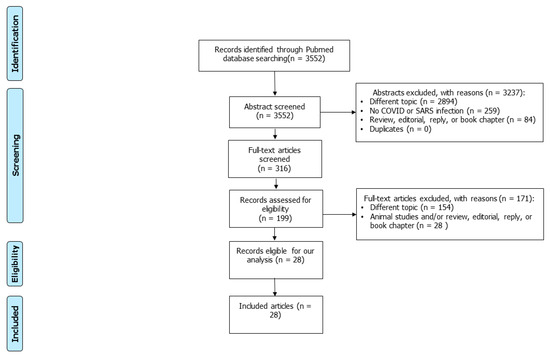
Figure 1
Open AccessArticle
Glycated Haemoglobin (HbA1c) and Future Physical and Mental Functional Health in the European Prospective Investigation into Cancer (EPIC)-Norfolk Population-Based Study
J. Pers. Med. 2023, 13(9), 1336; https://doi.org/10.3390/jpm13091336 - 30 Aug 2023
Abstract
Little is understood about the relationship between glycated haemoglobin and future functional health in the general population. In this work, we aimed to assess if glycaemic control is associated with future physical and mental functional health at 18-month follow-up in a UK general
[...] Read more.
Little is understood about the relationship between glycated haemoglobin and future functional health in the general population. In this work, we aimed to assess if glycaemic control is associated with future physical and mental functional health at 18-month follow-up in a UK general population, in those with and without diabetes. This work was a cross-sectional study. Between 1995 and 1997, participants of the European Prospective Investigation into Cancer, Norfolk, attended a health check including blood testing for haemoglobin A1c (HbA1c) and completed a health and lifestyle questionnaire. Eighteen months later, self-reported physical and mental functional health were assessed using short form-36 (SF-36). Outcomes of interest included physical and mental component summary (PCS and MCS, respectively) scores of the SF-36. A total of 7343 participants (56% women, mean (SD) 58.1 ± 9.5 years) were eligible to be included, of whom 167 had prevalent diabetes. In our linear regression analysis, a higher HbA1c (mmol/mol) was found to be associated with a poorer PCS score (coefficient −0.15 (p < 0.0001)) at follow-up. After adjustment for comorbid conditions, including obesity, this association was no longer statistically significant. A higher HbA1c (mmol/mol) was associated with a better MCS score at follow-up; this finding was significant when adjusted for comorbid conditions (coefficient 0.029 (p < 0.05)). Our findings suggest that the association between a higher HbA1c and poorer physical functional health is explained by a higher BMI and comorbidity status in a general population. While higher HbA1c was found to be associated with higher mental functional health at follow-up, the magnitude of this association was small. Healthy responder bias and unmeasured confounding variables may have influenced this result; thus, it should be interpreted with caution.
Full article
(This article belongs to the Section Clinical Medicine, Cell, and Organism Physiology)
Open AccessBrief Report
Relationship between the Tokyo Guidelines and Pathological Severity in Acute Cholecystitis
by
, , , , , and
J. Pers. Med. 2023, 13(9), 1335; https://doi.org/10.3390/jpm13091335 - 30 Aug 2023
Abstract
Background: It is not well understood whether the severity of acute cholecystitis (AC) correlates with the extent of gallbladder (GB) inflammation or laboratory findings. This study aimed to assess whether the severity of AC, in accordance with the Tokyo Guidelines (TGs), is consistent
[...] Read more.
Background: It is not well understood whether the severity of acute cholecystitis (AC) correlates with the extent of gallbladder (GB) inflammation or laboratory findings. This study aimed to assess whether the severity of AC, in accordance with the Tokyo Guidelines (TGs), is consistent with the extent of GB inflammation on histopathological and laboratory findings, including microbiological isolation in blood and bile. Methods: The medical records of patients who underwent cholecystectomy for AC between January 2017 and May 2020 were reviewed. Demographic data, laboratory findings, the microbiologic culture of blood and bile, the extent of GB inflammation, and stone composition were compared in accordance with the TGs. Results: A total of 217 patients were divided into three groups of increasing severity—Grade I (n = 146), Grade II (n = 51), and Grade III (n = 20)—in accordance with the TGs. The Grade III group contained significantly older patients compared with the Grade I or Grade II groups (Grade I, 56.9 ± 13.9; Grade II, 64.3 ± 15.4; Grade III, 69.9 ± 9.9; p-value < 0.001). Patients in the Grade III group showed significantly higher levels of CRP, WBC, creatinine, and bilirubin and lower levels of platelets and albumin compared with the Grade I or Grade II group. As the grade of severity increased, the rate of microbiological isolation in blood (Grade I, 0% [0/146]; Grade II, 2.0% [1/51]; Grade III, 20% [4/20]; p-value < 0.001) and bile (Grade I, 19.9% [29/146]; Grade II, 33.3% [17/51]; Grade III, 70% [14/20]; p-value < 0.001) also increased significantly. However, there were no significant differences in the extent of GB inflammation between grades. Conclusions: AC severity, as stated by the TGs, does not correlate with the extent of GB inflammation on histopathological and laboratory findings. However, microbiological isolation in blood and bile was increased proportionally to the grade of the TGs.
Full article
(This article belongs to the Section Clinical Medicine, Cell, and Organism Physiology)
Open AccessArticle
In Systemic Sclerosis Patients, Peripheral Blood CD21low B Cells and Serum IL-4 and IL-21 Influence Joint Involvement
by
, , , , , , and
J. Pers. Med. 2023, 13(9), 1334; https://doi.org/10.3390/jpm13091334 - 30 Aug 2023
Abstract
Systemic sclerosis (SSc) patients have an increased frequency of CD21low B cells and of serum interleukin-4 (IL-4) and IL-21, each possible markers of joint involvement in inflammatory arthritis. The aim of this study was to investigate the possible influence of CD21low
[...] Read more.
Systemic sclerosis (SSc) patients have an increased frequency of CD21low B cells and of serum interleukin-4 (IL-4) and IL-21, each possible markers of joint involvement in inflammatory arthritis. The aim of this study was to investigate the possible influence of CD21low B cells, IL-4, and IL-21 on joint involvement in a cohort of 52 SSc patients. The DAS28-ESR was correlated with CD21low B cells (r = 0.452, p < 0.001), IL-4 (r = 0.478, p < 0.001), and IL-21 (r = 0.415, p < 0.001). SSc patients with a DAS28-ESR > 3.2 had more CD21low B cells (12.65% (IQR: 7.11–13.79) vs. 5.08% (IQR: 3.76–7.45), p < 0.01), higher IL-4 levels (132.98 pg/mL (IQR: 99.12–164.12) vs. 100.80 pg/mL (IQR: 62.78–121.13), p < 0.05), and higher IL-21 levels (200.77 pg/mL (IQR: 130.13–302.41) vs. 98.83 pg/mL (IQR: 35.70–231.55), p < 0.01) than patients with a DAS28-ESR ≤ 3.2. The logistic regression analysis models showed that the DAI (OR: 2.158 (95% CI: 1.120; 4.156), p < 0.05) and CD21low B cells (OR: 1.301 (95% CI: 1.099; 1.540), p < 0.01), the DAI (OR: 2.060 (95% CI: 1.082; 3.919), p < 0.05) and IL-4 level (OR: 1.026 (95% CI: 1.006; 1.045), p < 0.01), and the DAI (OR: 1.743 (95% CI: 1.022; 2.975), p < 0.05) and IL-21 level (OR: 1.006 (95% CI: 1.000; 1.011), p < 0.05) were independently associated with a DAS28-ESR > 3.2. An elevated CD21low B cell percentage, IL-4 level, and IL-21 level was associated with higher articular disease activity in patients, suggesting a possible role in the pathogenesis of SSc joint involvement.
Full article
(This article belongs to the Special Issue New Biomarkers for Diagnosis and Therapy in Civilization Diseases)
►▼
Show Figures
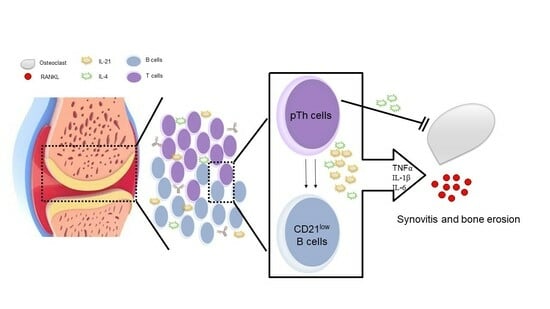
Graphical abstract
Open AccessArticle
SARS-CoV-2 Infection, Vaccination and Risk of Death in People with An Oncological Disease in Northeast Italy
by
, , , , , , , , , , , and
J. Pers. Med. 2023, 13(9), 1333; https://doi.org/10.3390/jpm13091333 - 29 Aug 2023
Abstract
People with a history of cancer have a higher risk of death when infected with SARS-CoV-2. COVID-19 vaccines in cancer patients proved safe and effective, even if efficacy may be lower than in the general population. In this population-based study, we compare the
[...] Read more.
People with a history of cancer have a higher risk of death when infected with SARS-CoV-2. COVID-19 vaccines in cancer patients proved safe and effective, even if efficacy may be lower than in the general population. In this population-based study, we compare the risk of dying of cancer patients diagnosed with COVID-19 in 2021, vaccinated or non-vaccinated against SARS-CoV-2 and residing in Friuli Venezia Giulia or in the province of Reggio Emilia. An amount of 800 deaths occurred among 6583 patients; the risk of death was more than three times higher among unvaccinated compared to vaccinated ones [HR 3.4; 95% CI 2.9–4.1]. The excess risk of death was stronger in those aged 70–79 years [HR 4.6; 95% CI 3.2–6.8], in patients with diagnosis made <1 year [HR 8.5; 95% CI 7.3–10.5] and in all cancer sites, including hematological malignancies. The study results indicate that vaccination against SARS-CoV-2 infection is a necessary tool to be included in the complex of oncological therapies aimed at reducing the risk of death.
Full article
(This article belongs to the Special Issue Cancer Challenges during COVID-19 Pandemic)
►▼
Show Figures

Figure 1

Journal Menu
► ▼ Journal Menu-
- JPM Home
- Aims & Scope
- Editorial Board
- Reviewer Board
- Topical Advisory Panel
- Instructions for Authors
- Special Issues
- Topics
- Sections & Collections
- Article Processing Charge
- Indexing & Archiving
- Editor’s Choice Articles
- Most Cited & Viewed
- Journal Statistics
- Journal History
- Journal Awards
- Editorial Office
Journal Browser
► ▼ Journal BrowserHighly Accessed Articles
Latest Books
E-Mail Alert
News
Topics
Topic in
Biomedicines, JCM, JPM, Reports, Toxins, Uro
Clinical, Translational, Basic Researches, and Application of Bacterial Toxins on Bladder Diseases and Lower Urinary Tract Dysfunctions
Topic Editors: Hann-Chorng Kuo, Yao-Chi Chuang, Chun-Hou LiaoDeadline: 30 September 2023
Topic in
Cancers, Cells, Current Oncology, JCM, JPM
Upper Aerodigestive Tract Cancer
Topic Editors: De-Chen Lin, Uttam K. SinhaDeadline: 20 December 2023
Topic in
Biomedicines, Cancers, JCM, JPM, Neurology International
Cancer Immunotherapies: From Laboratory to Clinical Studies
Topic Editors: Alessandra Carcereri De Prati, Zong Sheng GuoDeadline: 31 December 2023
Topic in
Healthcare, IJERPH, JCM, JPM, Applied Sciences, Technologies
Smart Healthcare: Technologies and Applications
Topic Editors: Gang Kou, Shuai Ding, Li Luo, Tian Lu, Yogesan KanagasingamDeadline: 20 January 2024

Conferences
Special Issues
Special Issue in
JPM
Selected Papers from the 2nd Conference with International Participation “Basic Research in Endocrinology: A Modern Strategy for the Development and Technologies of Personalized Medicine”
Guest Editors: Yuliya I. Ragino, Oksana D. RymarDeadline: 5 September 2023
Special Issue in
JPM
Cancer Biomarker Research and Personalized Medicine 2.0
Guest Editors: James Meehan, Mark E. GrayDeadline: 15 September 2023
Special Issue in
JPM
Personalized Prevention of Gallbladder Cancer
Guest Editors: Justo Lorenzo Bermejo, Dominique SchererDeadline: 25 September 2023
Special Issue in
JPM
Genetics, Genomics, and Precision Medicine in Colorectal Cancer
Guest Editors: Enrico Mini, Stefania NobiliDeadline: 20 October 2023
Topical Collections
Topical Collection in
JPM
Personalised Medicine–Bringing Innovation to the Healthcare System
Collection Editors: Denis Horgan, Gordon McVie
Topical Collection in
JPM
Genomic Medicine and Policy
Collection Editors: Christine Lu, Kurt Christensen, Nina Sperber
Topical Collection in
JPM
Advances of Emergency and Intensive Care
Collection Editor: Catalina Lionte